Cipro Resistance: Causes, Trends, and Global Impact
How Ciprofloxacin Lost Its First-line Effectiveness
Clinicians watched a reliable cure erode as resistant strains spread through hospitals and communities. Once-potent drugs failed more often, prompting frantic switches to broader agents. The narrative is one of evolutionary pressure, misuse, and slow recognition that change had occured.
Community prescribing, over-the-counter access in some regions, and inadequate dosing created a perfect storm. Laboratory surveillance lagged, so by the time resistance patterns were clear, treatment guidelines were out of date. Mutant bacteria exploited every gap to aquire survival advantage.
The result: common infections grew harder to treat, costs rose, and clinicians faced tougher choices. Reversing this trend requires stewardship, rapid diagnostics, and global coordination to limit further erosion of antibiotic efficacy and public education.
Genetic Mechanisms Driving Fluoroquinolone Resistance Worldwide

Microbes have learned to evade cipro’s bite through mutations that alter drug targets. Single nucleotide changes in DNA gyrase and topoisomerase IV reduce drug binding, while plasmid-mediated qnr proteins shield enzymes and promote survival.
Efflux pumps actively expel fluoroquinolones, and porin modifications decrease entry; together these mechanisms create high-level resistance that spreads quickly. Horizontal gene transfer lets resistance travel across species and borders, turning hospital outbreaks into regional threats.
Genomic surveillance reveals hotspots and evolutionary paths, but sequencing gaps and the complex interplay of mutations make prediction Definately hard. Addressing this requires coordinated stewardship, rapid diagnostics, and investment in research to outpace bacterial adaption. Global collaboration, funding, and policy change are urgently neccessary now today.
Human Behavior and Healthcare Practices Fueling Drug Failure
On a crowded clinic morning a man recalled how cipro stopped working for him after he abandoned therapy when symptoms eased, seeding resistant bacteria in his gut and among family members through everyday contact and neighbors.
Clinicians, pressed for time and faced with diagnostic uncertainty, often prescribe broad-spectrum drugs empirically. Lack of antimicrobial stewardship, pressure to satisfy patients, and easy refill policies amplify misuse and accelerate resistance at population level globally too.
In hospitals poor infection control, crowded wards, and inconsistent dosing protocols let resistant strains flourish. Subtherapeutic doses, unadjusted renal dosing, and unnoticed drug interactions can convert treatable infections into stubborn, expensive outbreaks nationwide quickly.
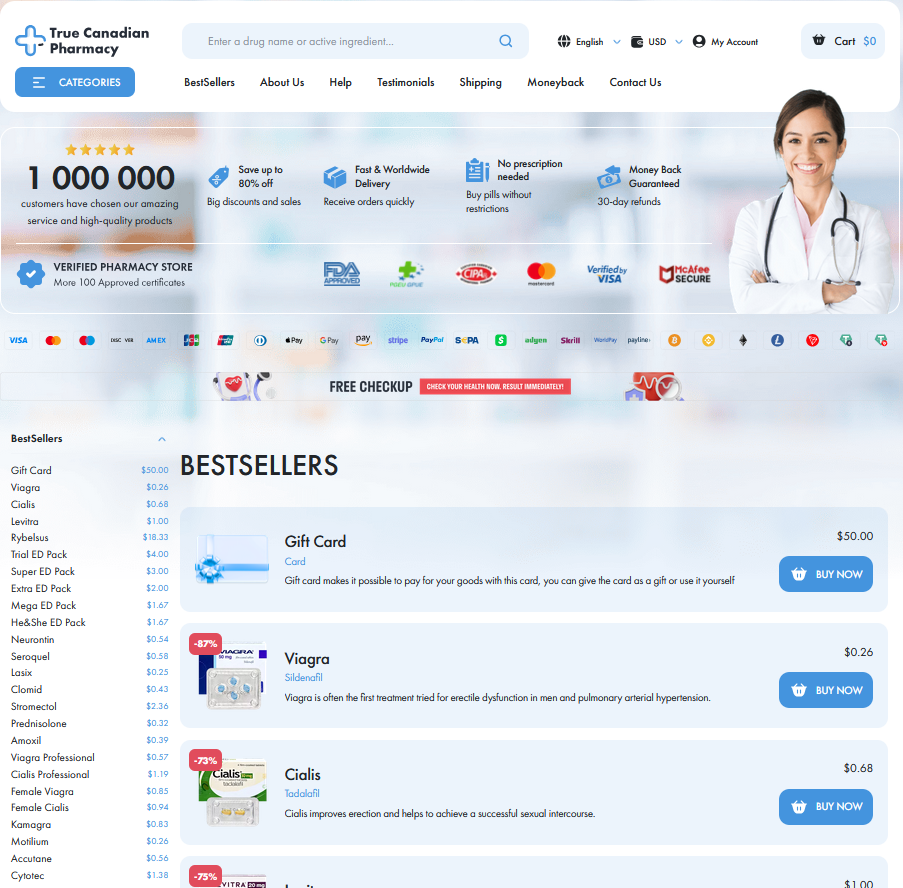
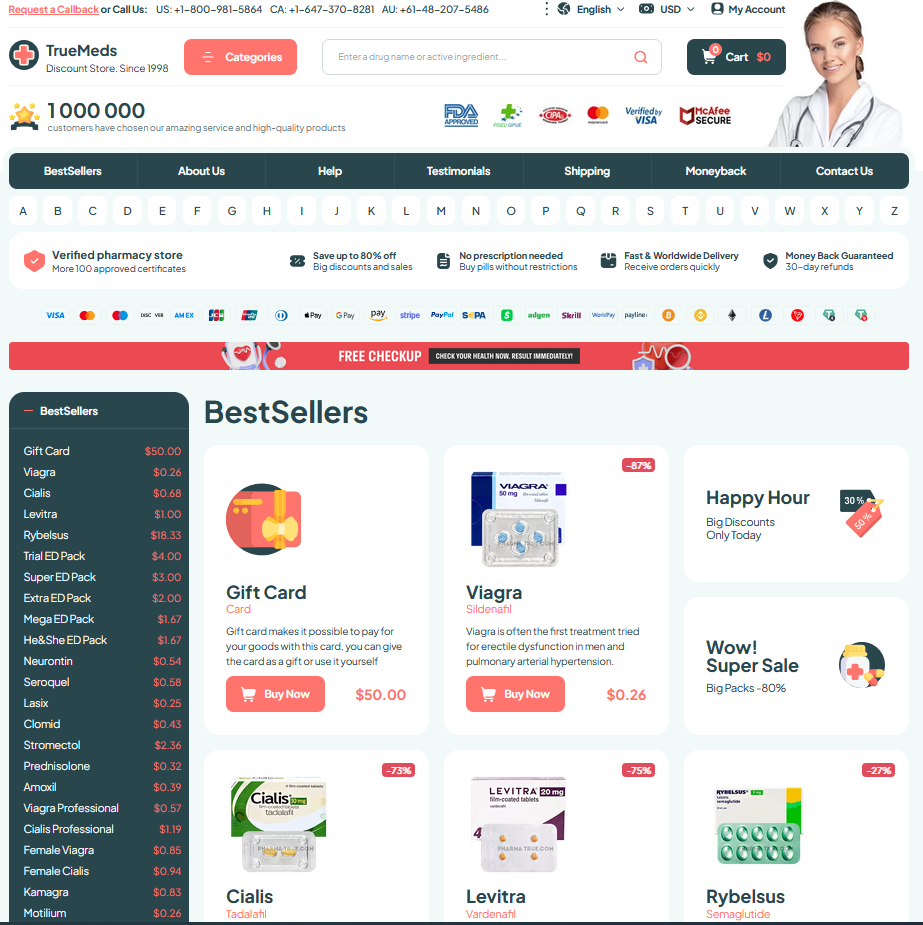
Easy OTC access in some regions, leftover pills shared among friends, and online pharmacies selling antibiotics without prescription propagate misuse. Public education, strict prescribing rules, and robust stewardship programs are indispensible to reverse trends.
Agricultural Use and Environmental Reservoirs Amplifying Resistance

Farmers once saw antibiotics as simple insurance; repeated dosing in livestock and crop protection has left soils and waters teeming with resistant strains. Runoff carries plasmids and mutations that render drugs like cipro less effective, creating ecological hotspots where resistance breeds and spreads silently.
Effluent from factories and poorly treated wastewaters seed rivers and sediments, forming an Enviroment reservoir where mobile genes transfer across species. Policy gaps and weak stewardship mean these reservoirs persist, demanding coordinated surveillance, reduced agricultural use, and stricter waste managment to curb the tide with urgency.
Surveillance Gaps and Diagnostic Challenges Masking True Burden
Hidden data and sporadic testing leave clinicians guessing about local trends, so cipro failures are often flagged late.
Surveillance networks exist, but underfunding and variable reporting mean national statistics can misrepresent outbreaks.
Rapid diagnostics would reveal resistance mechanisms early, yet many settings depend on empirical treatment and send no samples.
Patients travel, antibiotics circulate in communities, and environmental reservoirs hide resistant strains; without harmonized diagnostics the true burden becomes a patchwork. Occassionally weak laboratory links or Goverment secrecy create blind spots. Investment in lab networks, data-sharing platforms and clinician training would turn anecdote into evidence. Policymakers must fund standardized methods and real-time reporting so interventions target hotspots, preserve remaining cipro options, and avert wider crises.
Global Health Consequences and Policy Responses Needed Now
Clinicians face dwindling options as ciprofloxacin fails; routine urinary and bloodstream infections now demand broader, costlier therapies and longer daily hospital stays.
Public health systems grapple with outbreaks that spread faster when first-line drugs lose potency, amplifying mortality risks disrupting vaccination, essential care programs.
Low-income countries suffer disproportionally; limited access to diagnostics prevents timely stewardship, while weak surveillance masks true burden and hinders global response coordination.
Urgent policy actions include stewardship mandates, investment in rapid testing, phased agricultural antibiotic bans, and monitoring of the enviroment to avert global crisis. PubChem Ciprofloxacin CDC Antibiotic Resistance Threats